
Exploring Shiitake Mushroom Market Opportunity, Latest...
The Global Shiitake Mushroom Market size was valued at around USD 810 Milli...
-

The Global Shiitake Mushroom Market size was valued at around USD 810 Milli...

Shillong Teer Result Today and Khanapara Teer Common Number

A Look at Pakistan's Unique Take on Modesty and Style

Appointment Setter helps coaches book qualified sales calls, save time, and...
Discover essential Vastu Shastra tips from expert Vastu consultants in Gurg...

Discover luxury portable bathroom rentals for weddings, parties, and events...
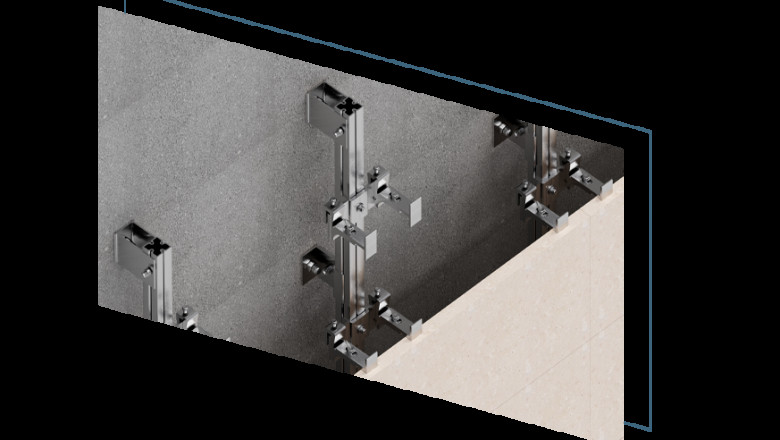
Denplex: Leading facade fixing company in Dubai, UAE. Expert solutions for...
Starting as a modest agency with a clear goal of helping businesses grow on...











